
Published: June 02, 2020
Chronic Obstructive Pulmonary Disease (COPD)
For those diagnosed with chronic lung disease, every breath can be a struggle. These patients experience inflammation to the airways that mimic the feeling of breathing through a straw, making it difficult to maintain enough energy and lung function to perform daily activities, among other debilitating symptoms. One of the most prevalent lung diseases is COPD, affecting nearly 30 million people in the United States.
Common among smokers, COPD is a group of chronic inflammatory lung diseases, such as emphysema and bronchitis, which cause difficulty breathing, cough, mucus production, and wheezing. Damage to the lungs caused by COPD occurs slowly over many years and worsens over time. Smoking is responsible for 85% – 90% of COPD Cases. While the damage is irreversible, patients who stop smoking may be able to regain some of their lung function, decrease inflammation in their respiratory tract, and improve their overall immune system.
COPD includes:
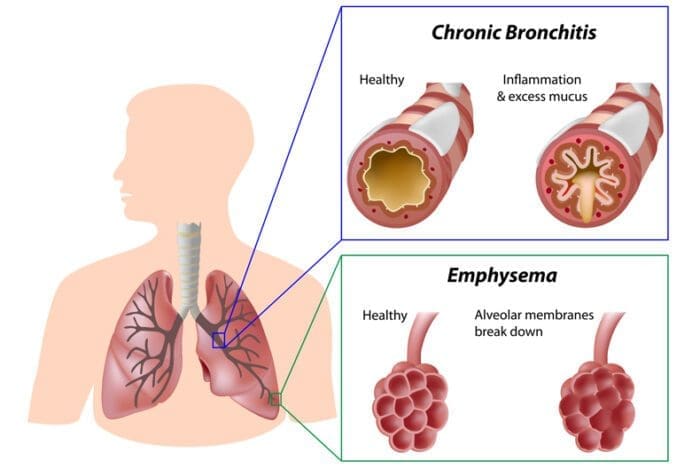
- Emphysema – A condition in which the air sacs of the lungs are damaged, stretched and enlarged.
- Chronic (long-term) Bronchitis – A condition in which the airways, or bronchial tubes, that move air to and from your lungs become inflamed and irritated.
Symptoms
Early symptoms include:
- occasional shortness of breath, especially after physical exercise
- recurrent mild cough
- clearing the throat often, especially first thing in the morning
- patients may avoid physical activities, such as taking the stairs
Symptoms can get progressively worse and harder to ignore. As the lungs become more damaged, you may experience:
- shortness of breath, after even mild exercise such as walking up a flight of stairs
- wheezing
- chest tightness
- chronic cough, with or without mucus
- clearing mucus from your lungs every day
- frequent colds, flu, or other respiratory infections
- lack of energy
Treatment
- Medications that help relax the muscles of the airways, widening the airways so you can breathe easier. They’re usually taken through an inhaler or a nebulizer. Additional medications (Glucocorticosteroids) can be added to reduce inflammation in the airways.
- To lower risk of other respiratory infections, your doctor may recommend getting a yearly flu shot, pneumococcal (bacterial infection) vaccine, and a tetanus booster that includes protection from pertussis (whooping cough).
- If the patient’s blood oxygen level is too low, they can receive supplemental oxygen through a mask or nasal cannula to help them breathe better. A portable unit can make it easier to get around.
- If all other treatments have failed, surgery may be an option. One type of surgery is called bullectomy. During this procedure, surgeons remove large, abnormal air spaces (bullae) from the lungs.
Another type of surgery is lung volume reduction surgery, which removes damaged upper lung tissue.
It is never too late to slow the progression of lung disease and improve your lung function. According to Dr. James D. Heddleson, Avita Pulmonologist and Critical Care Physician, “Studies indicate that lung function can improve after smoking cessation and with appropriate therapies. Our goal is to decrease the patient’s symptoms and improve their quality of life.”
For those who suffer with COPD, there are options to improve your breathing and decrease the risk of more serious complications, such as collapsed lung. Treatment options may include the use of medications, inhalers, oxygen therapy, and pulmonary rehabilitation. For more information about pulmonology at Avita, visit our pulmonary medicine page. To schedule an appointment call, 419-462-4588, or find a doctor.
Sources: Centers for Disease Control and Prevention, American Lung Association